Hospice Eligibility Guidelines for End-Stage Liver Disease
Download a PDF of these guidelines.
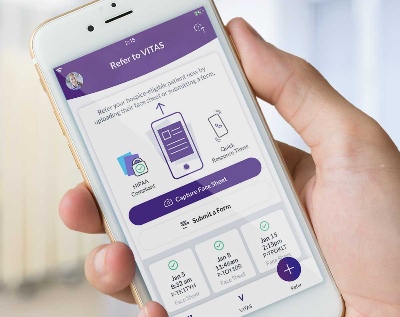
Are you a patient, family member, or caregiver? Learn about how VITAS can help patients with end-stage liver disease.
The term "liver disease" encompasses many diseases and disorders that cause the liver to function improperly or stop functioning. Abdominal pain, jaundice of the skin or eyes, or abnormal results of liver function tests suggest liver disease.
End-stage liver disease (ESLD) is an irreversible condition that leads to the imminent complete failure of the liver. Alcohol abuse is a major cause of ESLD in the United States and most Western countries. Cirrhosis, viral hepatitis, genetic disorders, cancer of the liver, autoimmune disorder, obesity, and toxins and drugs can be factors of ESLD and liver failure.
Without a liver transplant, patients with end-stage liver disease have a low life expectancy. They and their caregivers face significant physical and psychosocial challenges.
When Is Your Liver Disease Patient Eligible for Hospice Services?
Physicians may use clinical guidelines to identify patients in the final six months of liver disease. When it comes to end-of-life care, patients should be physiologically and psychologically hospice-appropriate.
In essence, liver disease patients are appropriate for hospice care if, despite adequate medical management, they suffer from persistent symptoms of hepatic failure, such as ascites, hepatic encephalopathy or recurrent varicella bleeding, and meet many of the following guidelines:
- Multiple hospitalizations, ED visits or increased use of other healthcare services
- Serial physician assessments, laboratory or diagnostic studies consistent with disease progression
- Multiple active comorbid conditions
Functional decline:
- Loss of functional independence
- Weight loss and/or reduced oral intake
- Unable to work
- Mainly sit or lie
- Confusion, cognitive impairment
Progressive symptoms not responsive to medical management, or due to patient noncompliance, including:
- Ascites, refractory to sodium restriction and diuretics, especially with associated spontaneous bacterial peritonitis
- Hepatic encephalopathy refractory to protein restriction and medical management
- Recurrent variceal bleed despite therapeutic interventions
- Hepatorenal syndrome
Laboratory indicators:
- Protime five seconds more than control or INR > 1.5
- Serum albumin ≤ 2.5 g/dL
Other factors:
- Transplant patient whose transplant has failed and patient is not eligible for or refuses another transplant
- Progressive malnutrition
- Muscle wasting with reduced strength and endurance
- Continued active ethanol intake (>80g ethanol per day)
- HBsAg-positive
VITAS provides these guidelines as a convenient tool. They do not take the place of a physician's professional judgment.
Source:
Wright JB, Kinzbrunner BM: "Predicting Prognosis: How to Decide when End-of-Life Care Is Needed." Chapter 1 in Kinzbrunner BM, Policzer J: End-of-Life Care : A Practical Guide. New York: McGraw Hill, 2011. Print.