VITAS Advantage: Case Study on High-Acuity Care for Physicians
Case Study: Patient with Advanced Alzheimer’s
RK*, an 87-year-old woman with advanced Alzheimer’s and two previous hospitalizations for pneumonia, experiences shortness of breath and aspiration pneumonia at home, where her daughter is her primary caregiver. During a same-day telehealth conference, RK’s physician and the daughter discuss the patient’s advance directives and goals of care; together they agree on an immediate hospice evaluation by VITAS.
Within two hours, RK is evaluated by a hospice admissions nurse and admitted to VITAS for hospice care at home, in accordance with RK’s wishes to avoid aggressive care near the end of life. VITAS delivers a hospital bed, pressure mattress, medications/supplies, and other diagnosis-specific equipment to the home later that day.
Over the next 3 weeks, RK receives regular visits from a hospice aide, respiratory therapist, and registered nurse to manage her symptoms and adjust medications. A hospice physician oversees her individualized care plan. Several times, temporary shifts of VITAS Intensive Comfort Care® are initiated to address exacerbations that include dehydration, delirium/agitation, dysphagia, and fever. A social worker and chaplain visit weekly to provide psychospiritual support to RK’s daughter and help her with anticipatory grief over her mother’s ongoing decline.
During the fourth week of hospice care, RK dies peacefully at home with her daughter at her side.
*These initials represent an anonymized patient and are used for the purposes of education only.
End-of-Life Care Trends Include Increasing Complexity of Care Needs and Rising Hospice Use
A review of data on epidemiology and care patterns at the end of life published in Health Affairs highlights recent trends in the way Americans are dying. Among the key findings is rising multimorbidity among Americans that impacts their end-of-life care.
Multimorbidity combined with functional limitations, such as frailty and cognitive impairment, is now considered the key indicator of the complexity of a patient’s end-of-life care—and a common challenge for healthcare providers, according to research. Multimorbidity in dying patients can result in conflicting treatment recommendations, higher costs, a greater burden on family caregivers, and more aggressive care—such as hospital and ICU admittance, which can conflict with the patient’s and family’s goals of care.
The authors stress that it is crucial for healthcare providers to address and consider the treatment of a patient’s comorbid conditions. Care that focuses only on what is required for a patient’s primary diagnosis at the end of life “misses the mark on the necessary resources and expertise of healthcare providers and caregivers to care for them,” they write.
Another major trend noted by the research team is that more Americans are dying at home or in an inpatient hospice facility, and fewer are dying in the hospital.
Research shows that most Americans prefer to die at home and to avoid intensive care at the end of life. "Transitions to the hospital at the end of life can lead to non-beneficial interventions, medical errors, injuries, increasing disability, worsening function, and adverse reactions for patients," the authors point out.
Hospice use has risen from approximately 10% of decedents in the 1990s to approximately 50% in 2014. From 1999 to 2015:
- The proportion of decedents dying in a hospital decreased from over 50% to 30%.
- The percentage who died at home rose from less than 25% to 30%.
- The proportion dying in an inpatient hospice facility rose from 0% to 8%.
While more Americans are turning to hospice, the authors report that hospice is often used as an “add on,” within days of death, after the extensive use of other healthcare services defined by increasingly aggressive care.
“This changing epidemiology of those in the last phase of life puts new pressures on the Medicare hospice benefit to ensure the availability of high-quality end-of-life care,” say the authors, who also call for a greater awareness of patients’ complex end-of-life care needs and earlier referral to hospice so patients can benefit from the full multidisciplinary care that hospice provides.
The VITAS Advantage: Higher Levels of Care Address Disease Exacerbations
VITAS supports physicians whose hospice-eligible patients require higher levels of care to manage disease exacerbations and progressions when medically necessary. Intensive Comfort Care® provides clinical support in the patient's home in shifts of care per Medicare guidelines. A short stay in an inpatient setting, staffed 24/7/365, is also available when symptoms cannot be controlled at home.
These extra levels of care support patients and physicians by:
- Ensuring that the end-of-life care patients receive is the care they prefer
- Reducing unnecessary and unwanted interventions and aggressive care for patients who prefer to die with comfort-only care at home or in their preferred care setting
- Delivering complex modalities to patients who require high-acuity care in their preferred setting, including comfort-focused medications, pain and fluid management, respiratory therapy, antibiotics, cardiac mediations, etc.
- Reducing hospital and ED admissions/readmissions and in-hospital mortality
Source: Aldridge, M. & Bradley, E. (2017) Epidemiology and Patterns of Care at the End of Life: Rising Complexity, Shifts in Care Patters and Sites of Death. Health Affairs, 38(9), 937-943. DOI: 10.1200/ JCO.18.02235
Is your patient ready for hospice?
Meet the VITAS Hospice Team

Physician
The physician closely monitors the progression of the patient’s illness, prescribes appropriate medications and coordinates care with other members of the team.
Hospice Nurse
The hospice nurse is skilled in assessing and managing pain and other symptoms. A nurse may also help with personal care.
Hospice Aide
Hospice aides provide personal care to the patient. They are also the “eyes and ears” for the rest of the hospice team.
Social Worker
The social worker acts as a friendly and skilled listener and provides emotional support.
Volunteer
The hospice volunteer can bring music or a Paw Pals animal companion, and spends quality time with the patient and family.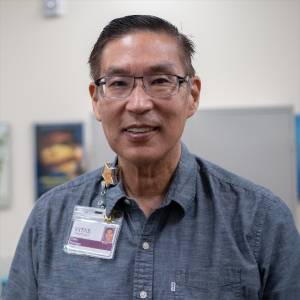
Chaplain
The chaplain ministers to the spiritual needs of patients and families of all faiths, and can work with their clergy.