Palliative Care vs. Hospice Care: Differences & Commonalities
Download a Guide: Hospice vs. Palliative Care
On This Page:
- Hospice vs. palliative care definitions
- Hospice vs. palliative care eligibility
- Hospice and palliative care teams
- Paying for hospice vs. palliative care
- Where do I receive hospice or palliative care?
- What kind of patients choose palliative care?
- Hospice vs. palliative care FAQ
What Is the Difference Between Palliative Care and Hospice Care?
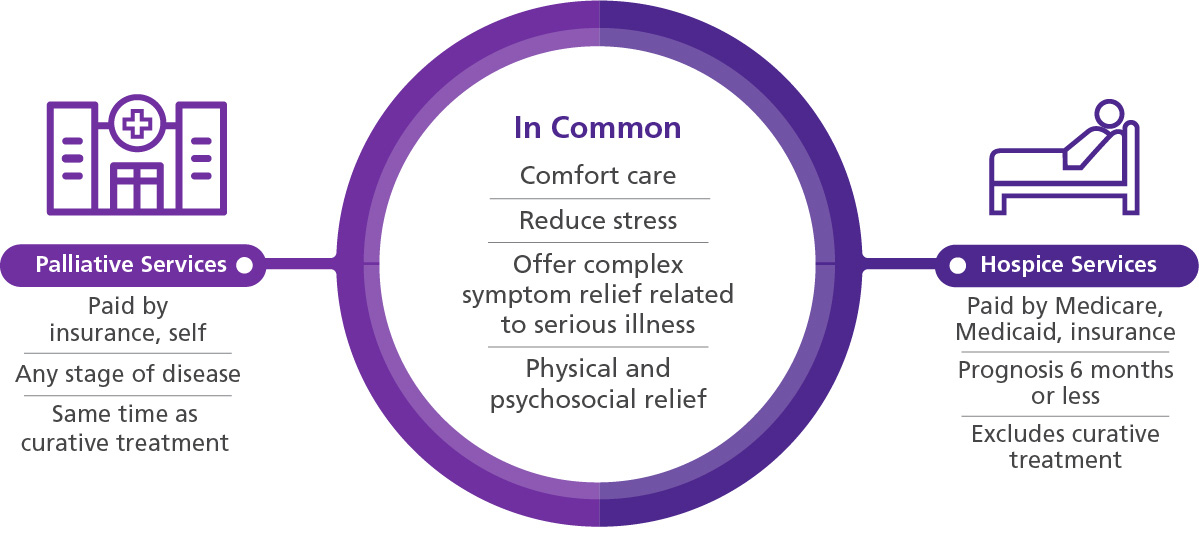
While the objective of both hospice and palliative care is pain and symptom relief, the prognosis and goals of care tend to be different. Hospice is comfort care without curative intent; the patient no longer has curative options or has chosen not to pursue treatment because the side effects outweigh the benefits. Palliative care is comfort care with or without curative intent.
Hospice care is similar to palliative care, but there are important differences. Because more than 90 percent of hospice care is paid for through the Medicare hospice benefit, hospice patients must meet Medicare’s eligibility requirements; palliative care patients do not have to meet the same requirements.
Hospice vs. Palliative Care Definitions
Hospice Care Definition
The definition of hospice care is compassionate comfort care (as opposed to curative care) for people facing a terminal illness with a prognosis of six months or less, based on their physician’s estimate if the disease runs its course as expected.
Palliative Care Definition
The definition of palliative care is compassionate comfort care that provides relief from the symptoms and physical and mental stress of a serious or life-limiting illness. Palliative care can be pursued at diagnosis, during curative treatment and follow-up, and at the end of life.
Hospice vs. Palliative Care Eligibility
Hospice eligibility requires that two physicians certify that the patient has less than six months to live if the disease follows its usual course. Palliative care eligibility has less firm guidelines and begins at the discretion of the physician and patient at any time, at any stage of illness, terminal or not.
Hospice and Palliative Care Teams
Interdisciplinary teams deliver both hospice and palliative care. They address physical, emotional and spiritual pain, including such common worries as loss of independence, the well-being of the family and feeling like a burden.
Paying for Hospice vs. Palliative Care
Hospice care costs are paid 100 percent by Medicare, Medicaid and private insurance; hospice is the only Medicare benefit that includes pharmaceuticals, medical equipment, 24/7 access to care, nursing, social services, chaplain visits, grief support following a death and other services deemed appropriate by the hospice agency. By comparison, palliative care costs—from office visits to prescription charges—can vary. Read more about who pays for palliative care here.
What Kind of Patients Choose Palliative Care?
The American Society of Clinical Oncology has identified the characteristics of a patient who should receive palliative care but not curative treatment; these characteristics are applicable to patients with other diseases, too.
- The patient has limited ability to care for themself.
- The patient has received curative treatment and is no longer benefiting from it.
- The patient does not qualify for an appropriate clinical trial.
- There is no evidence that further treatment would be effective.
Hospice vs. Palliative Care FAQ
Is palliative care the last step before hospice?
No. It’s an important part of hospice. All hospice patients continue to receive palliative care as they approach the end of their lives; minimizing patients’ discomfort and providing symptom relief are daily priorities for hospice health providers.
This might be a helpful way to think about it: "All hospice care involves palliative care, but not all palliative care takes place in hospice."
Is palliative care the same as end-of-life care?
No. Although palliative care becomes important at the end of life, palliation is compatible with any prognosis.
A patient in chemotherapy deserves to be as comfortable as possible while pursuing curative treatment; a patient in hospice deserves the same comfort as they enter their last months of life.
Any treatment that improves quality of life and reduces symptom burden for either of these patients is palliative care.

How VITAS Can Help
With 40 years of leadership in hospice and palliative care, VITAS offers:
- Personalized care plans by patient's diagnosis
- Interdisciplinary care teams
- Therapy, emotional and pastoral support
- Grief and bereavement services
Call VITAS to learn how we can help you.
Call VITAS at 800.582.9533