How We Help Accountable Care Organizations
To help Accountable Care Organizations (ACOs) better serve patients who may be candidates for hospice care, VITAS offers ACO providers alternative resources that positively impact the quality of care, the patient experience and the overall cost of care.
VITAS specializes in helping our ACO partners manage advanced illness. We titrate care to the patient's current level of need, and we transition seriously ill patients to an appropriate secondary site of care, supported by care plans that include high-acuity and complex modalities.
Benefits of a Hospice Partnership for ACO Providers
VITAS can assist ACOs in the new Centers for Medicare and Medicaid Services (CMS) "Pathways to Success" Program, including Basic and Advanced models, along with Next Generation ACOs.
Our personalized care plans improve patients' quality of life, resulting in higher CAHPS and HEDIS scores. VITAS also impacts:
- Risk linked to specialized care for end-of-life patients
- Quality thresholds, including advance care planning and hospital readmission metrics
- Medicare per-beneficiary episode spending for hospice-eligible patients
- Reduced total cost of care for high-need, high-cost patients—populations that require complex and multi-faceted care
- Reduced leakage
- Comprehensive services and high-acuity care that mitigates the risk of readmission
- Routine cost forecasting for ACH/PGP prior to reconciliation
- Goals of care/advance care planning
- Hospital LOS and bed cycle challenges
- ED utilization
- CAHPS and HEDIS scores by supporting quality measures that:
- reduce hospital readmissions and in-house acute mortality rates
- improve patient/family satisfaction
- Patients with advanced disease and limited potential for restored functional dependence by providing a seamless system of care
- Clinician continuing education and patient/family education
- Expanded psychosocial resources
- Collaboration with patients’ physicians for individualized symptom management
Partnering with VITAS as the preferred hospice and palliative care partner enhances the success of your ACO. Through VITAS’ value-based care coordination, transition processes and our advanced iOS-based technology, hospice and palliative care patients receive individualized care. Timely hospice and palliative care can eliminate unnecessary acute care encounters and increase patient satisfaction.
Value-Based Care Requires a Collaborative Team-Based Approach
In tandem with the Institute for Healthcare Improvement's Triple and Quadruple Aims, ACOs involved in fee-for-service and commercial lines of business are being asked to improve the health of their patient populations, improve patients’ experiences and reduce the overall per-capita healthcare spending. Yet:
- Nearly 50 percent of US healthcare expenditures go to the “at-risk” 5 percent of the population1
- Chronic diseases are responsible for 7 in 10 deaths each year; treating patients with chronic diseases accounts for 86 percent of our nation's healthcare costs2
- In a national study, 15 percent of emergency department visits (about 1 in 7) were made by a patient who died within six months3
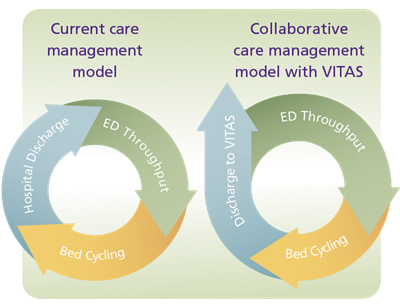
How VITAS Helps Break the Cycle
On average, one in five elderly patients discharged from the hospital is re-hospitalized within 30 days4. A referral of hospice-eligible patients to VITAS, bolstered by the time and attention of our individualized plan of care, helps break that cycle.
- Hospice care at home, wherever a patient calls home: private residence, nursing home, assisted living community or other residence for the elderly
- 24/7 clinical support with Telecare
- All levels of care—home, Intensive Comfort Care® (continuous home care) and inpatient care—customized to meet individual care management needs
- Comprehensive education programs for patients and families
- Specialized care, including multilingual staff, Jewish accreditation, veteran-centric care, music therapy, pet visits, illness-specific care plans, etc.
Sources:
- Cohen, SB, “The Concentration of Health Care Expenditures and Related Expenses for Costly Medical Conditions, 2012.” Medical Expenditure Panel Survey, Agency for Healthcare Research & Quality, 2014. https://meps.ahrq.gov/data_files/publications/st455/stat455.pdf
- The Dartmouth Atlas of Healthcare, http://www.dartmouthatlas.org/data/topic/topic.aspx?cat=18
- Smith A et. al. “Half Of Older Americans Seen In Emergency Department In Last Month Of Life; Most Admitted To Hospital, And Many Die There.” Health Affairs 2012; 6:1277-1285.
- Jencks, SB. “Rehospitalizations among Patients in the Medicare Fee-for-Service Program.” The New England Journal of Medicine. 360:1418-1428 April 2, 2011.