Choosing a Hospice Organization: Making Referrals That Most Benefit Your Patients
When your patient is seriously ill and hospice eligible, how do you know which hospice organization to refer to? Aren’t they nearly all the same?
All hospices must provide core services, but substantial variation exists in how hospices deliver these services. These differences can impact the quality of care for both the patient and their family or caregivers.
What is common for all US hospices is that the Medicare Hospice Benefit covers the costs of hospice services. Medicare Part A covers up to 100% of the costs related to a hospice-eligible patient’s terminal diagnosis, which indicates the patient has six months or less to live if the disease runs its typical course. Coverage includes everything involved in hospice care, from visits by a nurse, physician, and other healthcare professionals to therapy, medication, and supplies.
What to Expect: Core Hospice Services
Hospice is not a location. Team members can provide hospice care wherever the patient calls home—in a private residence, assisted living community, or skilled nursing facility. Common services that you can expect from most hospices include:
- Advance care planning assistance and resources
- Symptom management/pain relief that is not curative but enhances the patient’s quality of life
- Clinical care provided by an interdisciplinary team, including physicians and nurses along with the services of home health aides and social workers
- Emotional and spiritual support from bereavement specialists and/or chaplains for the patient and their families
- Four levels of hospice care, including routine home care, continuous home care for up to 24-hours-a day when medically needed, general inpatient care, and respite care for the caregiver
Yet key differentiators can distinguish hospice providers, including their ability to respond 24/7/365, their expertise with high-acuity care, and their care coordination, along with their track record for compassionate care.
The VITAS Advantage: Supporting Clinicians While Caring for Patients and Families
What happens if a patient has an accident or emergency in the middle of the night? Rather than going to the ED, suppose the hospice provider can respond with clinical care? VITAS does, specifically offering:
- 24/7/365 clinical care support, including telehealth with around-the-clock access to clinicians for triage, assessment, and treatment guidance. Seamless care transitions are available at any time of day or night.
- Care coordination that assesses and manages individualized patient care. VITAS interdisciplinary teams facilitate communication about patient care transitions, symptom management, health status, and quality of life.
- Open formulary for individualized care plans, including continuation of disease-directed medications. A VITAS nurse supervises medications and compliance to mitigate chances of return to hospital/ED.
- Complex modalities supported by physician/APRN home visits, aggressive symptom management: IV hydration/antibiotics, high-flow O2, Sub-Q Lasix, inotropic therapy, and more.
- High-acuity care for patients with acute symptoms; intensive symptom management that aligns with patient care goals. VITAS supports a reduction in overall healthcare costs and reduces likelihood of readmissions associated with alternative post-acute care settings.
- Advanced illness specialists who deliver customized educational plans based on practice needs and goals and clinical resources to enhance prognostication of advanced illness patients. Assist with goals-of-care conversations, specialist consults, medication reconciliation, and more.
- Cultural competency, embracing diverse backgrounds and perspectives of those with whom we work and the patients and families we serve, regardless of age, gender, gender identity, ability, education, ethnicity, nationality, political opinion, professional experience, race, religion, sexual orientation, and socioeconomic status.
Selecting a Hospice: Helping Families Prepare
Once you determine a patient is hospice eligible, how can you guide family members to prepare for the next step of accepting a referral to hospice care? You can ask questions like these to encourage them to meet with a potential hospice organization:
- Has your loved one talked to you or written down their wishes about care near the end of life?
- Less than 40% of Americans have not completed an advanced directive.
- Have you discussed where they would like to receive care in their last months, weeks, or days?
- 70% of the population would prefer to die at home.
- Only about 1/3 pass in their homes.
- Do you understand the four levels of hospice care?
- Who will be the main caregiver for your loved one at home?
- Have you discussed managing pain?
- Have you talked about the spiritual needs of your loved one and your family? Do you know that emotional support is available to both you and your loved one?
- Do you understand the Medicare Hospice Benefit and how hospice costs will be paid for?
It can be empowering to have options near the end of life. When a patient seeks a higher quality of life in their final months, weeks, and days, hospice may be their best choice. Selecting a hospice provider that can provide the 24/7/365 clinical support and compassionate care they need will enhance their experience—as well their caregivers’.

Check Hospice Guidelines
Get diagnosis-specific guidelines in our hospice eligibility reference guide.
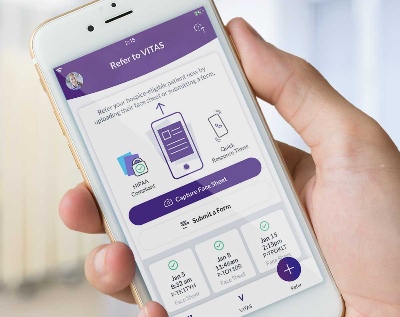
Hospice Guidelines by Diagnosis Refer Your Patient