By Joseph Shega, MD, EVP Chief Medical Officer, VITAS Healthcare
Today, an estimated 6.9 million Americans are living with Alzheimer’s or other dementias.1 Many of these individuals have a spouse, family member, or other loved one assisting them with daily care. These caregivers help them move in and out of bed, dress, bathe or shower, and provide feeding and bathroom assistance. They coordinate care with other family members and healthcare providers and offer emotional support. This time-intensive caregiving for an individual with advanced dementia averages about 92 hours per month.1
As their loved one’s illness progresses, these responsibilities can feel staggering, often leading caregivers to burn out. Studies show that people aged 65 and older survive an average of four to eight years after an initial diagnosis of Alzheimer’s, yet some live as long as 20 years.1 In another study, well over half (57%) of family caregivers of people with Alzheimer’s or other dementias provided care for four or more years.1
Stress on Alzheimer’s and Dementia Caregivers
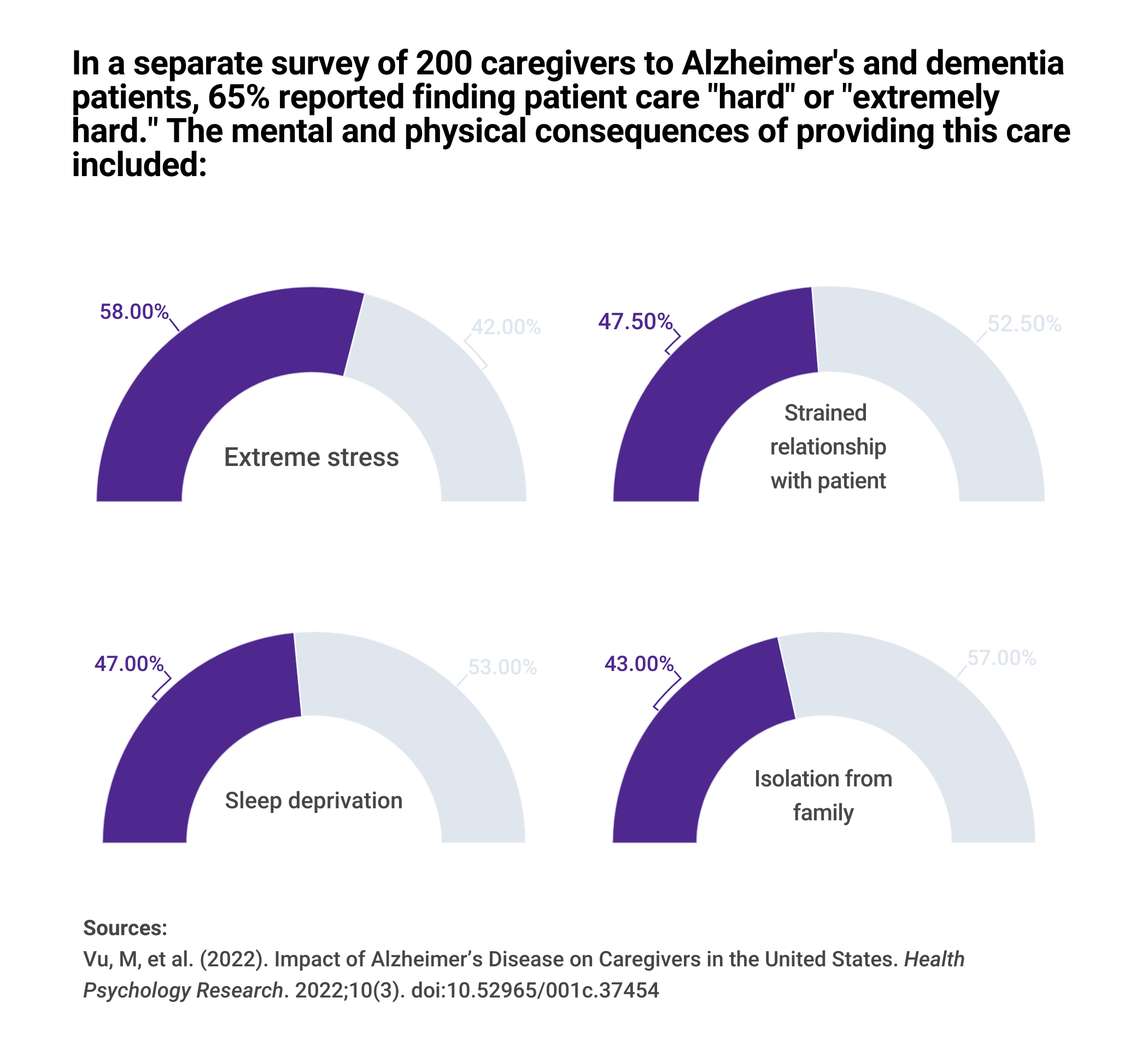
The long-term effects caregivers experience when managing symptoms and assisting with activities of daily living (ADLs) for individuals with Alzheimer’s or other dementias can be significant. In a survey of caregivers for Alzheimer's and dementia patients, 74% reported they were “somewhat concerned” to “very concerned” about maintaining their own health since becoming a caregiver. In 2021, it was estimated that dementia caregivers bore nearly twice the average out-of-pocket costs of non-dementia caregivers ($12,388 versus $6,667).1 The gradual progression of the disease causes an increase in stress and grief in caregivers, negatively impacting their physical, mental, and social health.2
Hospice Care: Relieving the Caregiving Burden
What offers relief?
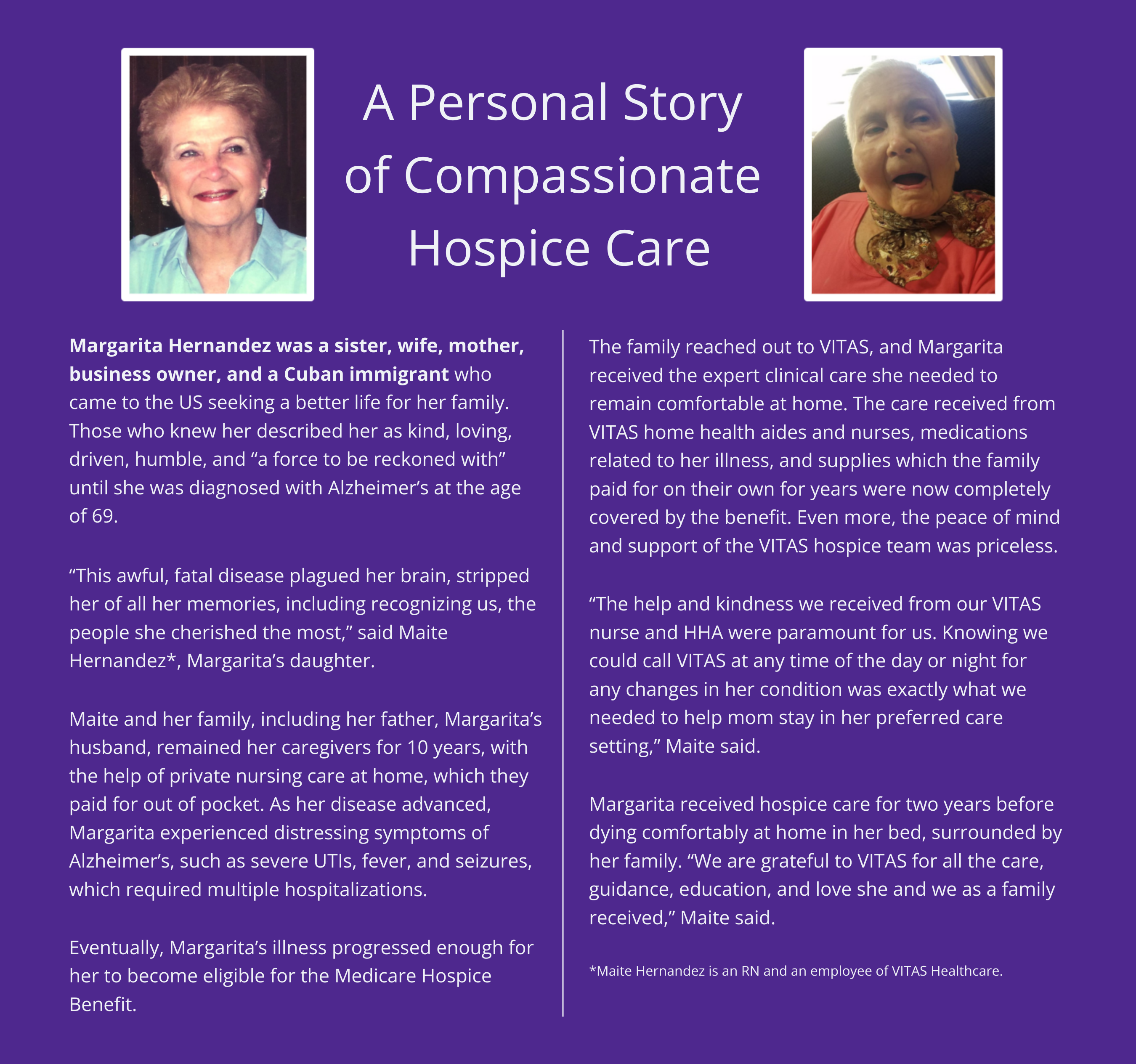
Hospice services have proven to ease the caregiver burden on family members and support the patient with a personalized disease-directed care plan. VITAS interdisciplinary care teams consisting of a physician, nurse, home health aides, bereavement specialist, and chaplain respond to the clinical, psychosocial, and spiritual needs of the patient. The Medicare Hospice Benefit covers hospice costs related to the terminal illness for eligible patients, including medications and home medical equipment. For people living with advanced dementia, research demonstrates the value of hospice:
- Hospice-enrolled people living with dementia had a higher quality of life compared to those without hospice.
- End-of-life transitions (e.g., hospitalizations, ED visits, etc.) were significantly lower for hospice enrollees compared to those who were not.
- Hospice beneficiaries saw a cost savings of $670 in the last month of life compared to non-hospice users. 3-4
When clinical care is accessible 24/7/365 and home health aides visit regularly to assist with activities of daily living (ADLs), caregivers no longer shoulder the full burden of care.
Caregivers who utilized hospice reported5:
- Increased satisfaction with care
- Decreased burden
- Decreased anxiety and depression
- Improved overall health
Leaning on experienced hospice care team members helps avoid caregiver burnout. Also, caregivers experienced less risk for PTSD with home hospice deaths as compared to the ICU, and home hospice reduced the risk for prolonged grief disorder compared to hospital deaths.6
Emotional Support: Dealing With Anticipatory Grief
VITAS grief and bereavement experts help caregivers, other family members, and the patient through the beginning stages of grief. Patients with advanced illnesses such as Alzheimer’s or dementia and their loved ones usually begin the grieving process before the actual loss occurs. This is called “anticipatory grief.”
Although it may be uncomfortable, anticipatory grief is sometimes helpful. It is a natural process that helps individuals prepare for emotional and physical closure. It is also a time when both patient and family prepare for change. Having expert support during this sensitive time can be comforting.
Drawing on the Full Support of Hospice Services
Helping caregivers navigate the challenges of advanced dementia is best before they experience burnout. VITAS is ready to assist hospice-eligible patients in improving their quality of life—and supporting family caregivers in maintaining theirs as well.
Learn more about Hospice Care for Alzheimer’s Disease and Dementia.
1 Alzheimer’s Association. (2024). Alzheimer's Association 2024 Alzheimer's Disease Facts and Figures. Retrieved 5/31/2024.
2 Vu, M, et al. (2022). Impact of Alzheimer’s Disease on Caregivers in the United States. Health Psychology Research. 2022;10(3). doi:10.52965/001c.37454
3 Harrison, et al. (2022). Hospice Improves Care Quality For Older Adults With Dementia In Their Last Month Of Life: Study examines hospice care quality for older adults with dementia in their last month of life. Health Affairs, 41(6), 821-830.
4 Aldridge, et al. (2022). Association between hospice enrollment and total health care costs for insurers and families, 2002-2018. JAMA Health Forum. 3(2), e215104-e215104.
5 Irwin, S., et al. (2013). Association Between Hospice Care and Psychological Outcomes in Alzheimer’s Spousal Caregivers. Journal of Palliative Medicine, 16(11), 1450-1454
6 Wright, et al. (2010). Place of death: correlations with quality of life of patients with cancer and predictors of bereaved caregivers' mental health. Journal of Clinical Oncology, 28(29), 4457.