The Many Gifts of Hospice: What Patients Can Receive Rather Than ‘Giving Up’
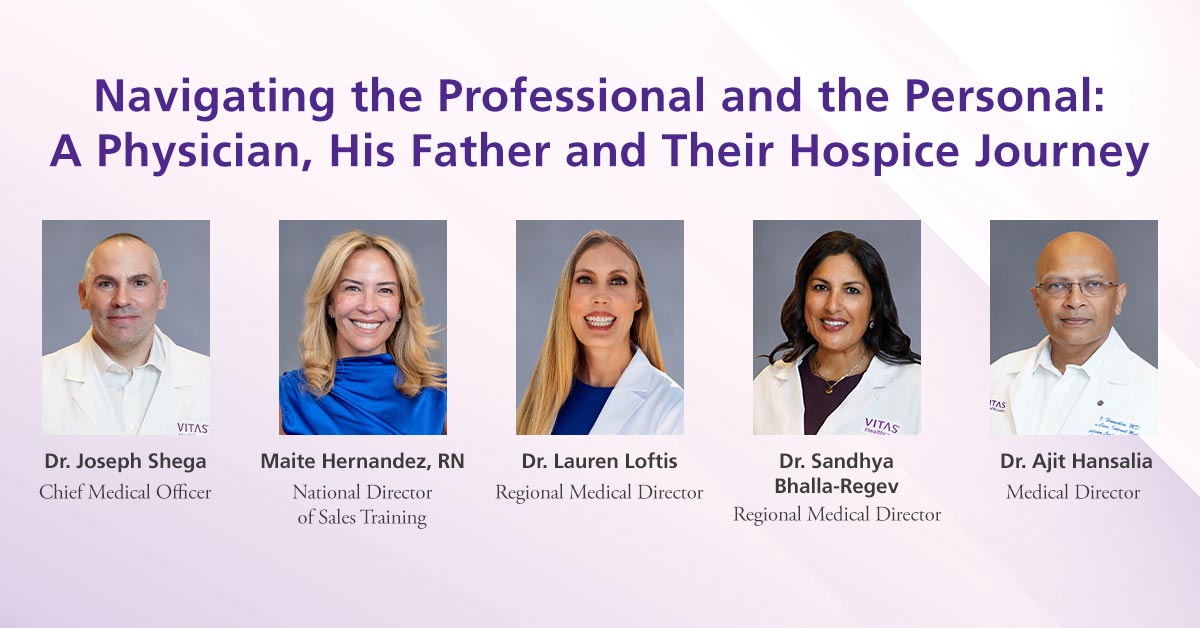
Regional Medical Directors Dr. Lauren Loftis and Dr. Sandhya Bhalla-Regev, Medical Director Dr. Ajit Hansalia, and National Director of Sales Training Maite Hernandez, RN, joined Executive Vice President and Chief Medical Officer Dr. Joseph Shega on November 6, 2024, for a panel discussing the hospice journey. Here is a summary of their presentation.
Hospice is commonly thought of as an option that is essentially ‘giving up.’ Yet once patients have exhausted avenues for curative care, hospice becomes a choice for increasing their quality of life instead. Patients receive 24/7 clinical support that helps manage pain and symptoms along with a full team of experts to provide interdisciplinary support. Hospice care allows seriously ill patients and their families to focus on what is most important to them in their final months, weeks, and days.
In 1982, the federal government established the Medicare Hospice Benefit for patients who have a prognosis of six months or less to live if their disease state runs its normal course. Common diagnoses for those with advanced illness who may qualify for hospice include cancer, Alzheimer’s/dementia and other neurological diseases, advanced cardiac disease, advanced lung disease, as well as other, less common conditions including ALS, sepsis, liver or renal disease, and HIV/AIDS.
One Physician’s Journey to Hospice With His Father: Seeing the Value in Real Time
As Dr. Joseph Shega relays, caring for his father with advanced cancer helped him see hospice through a more personal lens.
“After 11 years of anti-tumor treatment for stage 4 colorectal cancer, my dad had a myocardial infarction that further weakened him and led us to a goals-of-care conversation,” says Dr. Shega. “The anti-tumor treatments caused him to feel more and more fatigued. After additional hospitalizations for recurrent infections, he could no longer muster the energy or will to get to his baseline functional status. I asked him how he wanted to live during his remaining time.”
William Shega wanted to spend time at home, not pursuing acute care that would not likely prolong his life and only increase his suffering. He knew he was not getting stronger. Because hospice is the only post-acute setting that can titrate to the level of care needed without changing the care setting, Mr. Shega could remain at home surrounded by his wife and loved ones. Hospice services provided goal-directed palliative care, improved pain control, and increased Mr. Shega’s satisfaction.
With a team of experts to assist family caregivers in the day-to-day management of his symptoms, home medical equipment, and medications, and home health aides to help with activities of daily living, Mr. Shega received the care he was seeking in the comfort of his home.
Should he have needed a higher level of care, Mr. Shega had access to Intensive Comfort Care®, which enables continuous care for acute symptom management or inpatient care at a dedicated hospice inpatient facility if his symptoms became more than could be managed at home.
Also, if family caregivers are at risk of burnout, short-term respite care in a Medicare-certified hospital, hospice facility, or long-term care facility for up to five days is available.
With multiple levels of care and medical, psychosocial, and spiritual support, hospice offered the services that helped Mr. Shega spend time with his grandchildren and children.
“Hospice is a beautiful gift, giving autonomy and control back to the patient,” says Dr. Shega.
Treat Patients as You Would Family Members: Ask About Goals of Care
Without a goals-of-care conversation, physicians do not know what the patient prefers for their end-of-life journey and patients do not know all of their care options. Initiating these conversations allows patients and families to engage in advance care planning. Two approaches provide a framework for healthcare professionals to pursue this conversation:
- SPIKES is a mnemonic that incorporates an approach for the conversation and refers to Setting, Perception, Invitation, Knowledge, Emotion, and Summarize. Learn more about it here.
- ACACT helps clinicians work through common objections when talking about end-of-life care: acknowledge the difficult decision, clarify their concerns, answer questions, confirm the decision to choose hospice, transition to practical next steps.
Healthcare professionals can respond with clarity and accuracy and become more comfortable and skilled at addressing individual needs once they are prepared for common objections. Each of these approaches helps the clinician interact with patients and families empathetically.
Choosing a Better Ending
Hospice is not about death and dying. Mr. Shega’s story is one shared by countless families across the country. Patients with advanced cancer often reach a point where curative therapies become “palliative” therapies—medicine can’t cure the disease, but hospice can maximize their quality of life for as long as possible.
Often discontinuation of cytotoxic chemotherapies can actually reduce morbidity and help patients experience a better quality of life. By identifying hospice-eligible patients earlier, they receive the full breadth of services they are entitled to as their serious illness continues to progress.
One of the most important aspects of the Medicare Hospice Benefit is that hospice provides dedicated family and caregiver support and ongoing bereavement services prior to and after death for at least 13 months. Without hospice, most families go without these services and face loss alone.
To refer your hospice-eligible patient to VITAS, contact us at 800-582-9533.

