Although Physicians Agree End-of-Life Conversations Are Important, Fewer Than Half Feel Prepared
In a survey of physicians caring for older patients, 99% expressed the opinion that advance care planning (ACP) conversations with patients are important. Despite this, most physicians reported feeling uncomfortable about such conversations and believed that certain barriers often hindered them from initiating ACP discussions.
Researchers conducted a phone survey involving 736 actively practicing U.S. physicians (male, 81%; white race, 75%; age ≥ 50, 66%) regularly seeing patients age 65 and older, including 470 internists and primary care clinicians, 85 oncologists, 87 pulmonologists, and 94 cardiologists.
The survey questions elicited ACP opinions, experiences and perceived barriers to ACP conversations.
Researchers’ findings were published in the Journal of the American Geriatrics Society.
Key Facts: Physician Experiences
- 53% of respondents reported they were regularly seeing patients age ≥ 65 years who they "would not be surprised if they died within the next year."
- Only 29% of respondents reported having specific end-of-life (EOL) care conversation training.
- Only 14% of physicians caring for fee-for-service patients reported having billed Medicare for ACP conversations during the first year of the new benefit.
Although most reported having ACP and EOL conversations with patients, only 21% said they were doing so "frequently." Physicians with specific training and/or an assessment system in place were more likely to be having ACP conversations.
Physician Opinions and Priorities
Nearly all respondents (99%) reported feeling ACP conversations with patients are important; 51% considered them extremely important.
Physicians with EOL conversation training and/ or a formal assessment system were more likely to believe ACP conversations are extremely important.The difference in opinion was most pronounced among those with an assessment system; 61% of these physicians, compared to 47% of those without, described ACP conversations as extremely important (P < 0.05).
Respondents rated various motivating factors for having ACP discussions. The strongest motivators were honoring patients' values and wishes, which 92% cited as very or extremely important, and reducing unnecessary or unwanted hospitalizations.
Barriers to EOL Care Discussions
Interviewees were asked whether certain barriers had "ever gotten in the way of talking to [patients] about their [EOL] wishes." The most commonly cited barriers include:
- Lack of time (66% of respondents)
- Disagreements between patient and family (65%)
- Feeling unsure of timing (60%)
- Concerns the conversation might be uncomfortable (51%)
- Not wanting to lose hope (46%)
- Being unsure what's culturally appropriate (44%)
"Given the gap between what people want at the end of life and the care they receive, we need to build on available training tools and embed them systematically into practice," the authors state. They advocate for "broadly available" ACP conversation training and use of a formal assessment system.
SPIKES: A Method for Approaching EOL Conversations
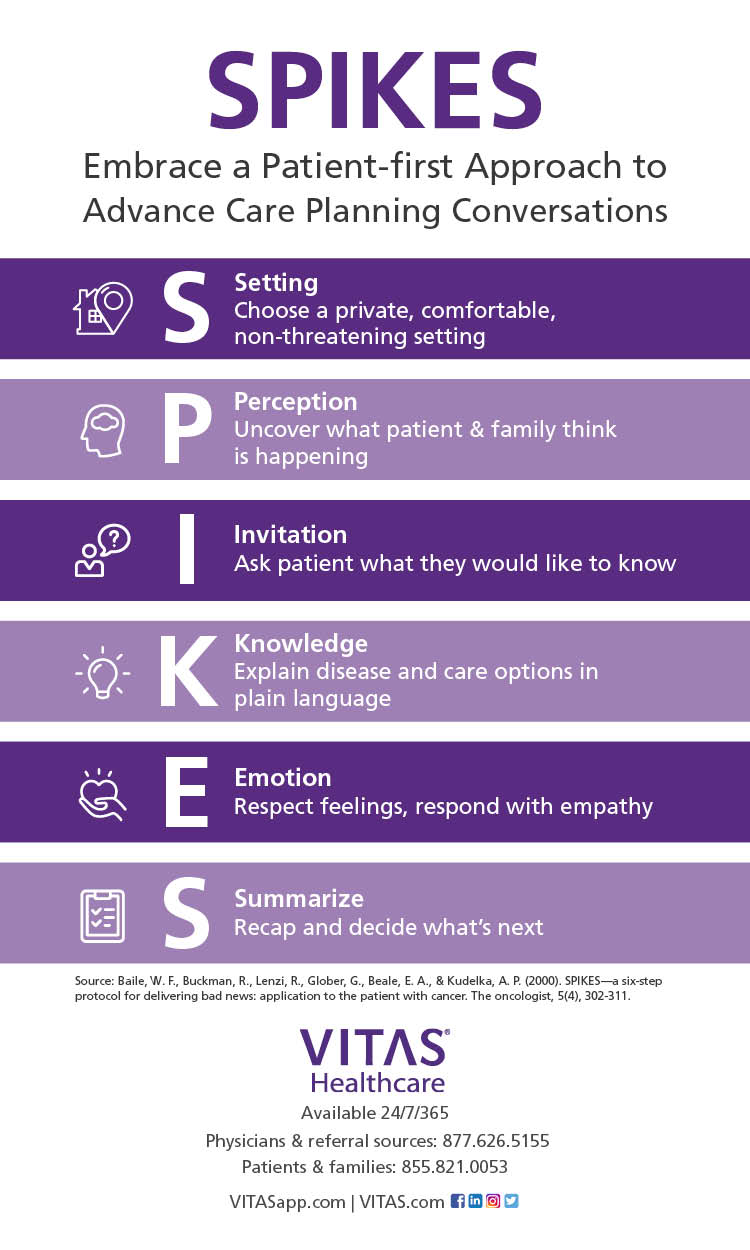
EOL experts recommend the SPIKES method for discussing hospice care with a patient:
- S=Setting: Choose a private setting where you can sit face-to-face with the patient and a family member or confidant. If the patient does not speak English, rely on a professional interpreter rather than a family member.
- P=Perception: Ask the patient how much they know, perceive or suspect before you begin the conversation.
- I=Invitation: Subtly invite the patient to provide clues about willingness to receive more information. Ask if they would like to talk about test outcomes, treatments, etc. If the patient does not respond favorably, suggest that you talk again later that day or the next. Then follow through.
- K=Knowledge: Share information directly and simple. After you've opened the conversation, stop talking. Listen to the patient's responses and emotions.
- E=Empathy: Identify with the patient's emotional reaction in a kind way that suggests you understand and appreciate their response and are concerned about their future.
- S=Summation: Summarize the news and recommend hospice care.
Learn More: Having EOL Conversations With Your Patient
Source: Fulmer T, et al. (2018). Physicians' Views on Advance Care Planning and End-of- Life Care Conversations. Journal of the American Geriatrics Society. DOI: 10.1111/ jgs.15374

Check Hospice Guidelines
Get diagnosis-specific guidelines in our hospice eligibility reference guide.
Hospice Guidelines by Diagnosis Refer Your Patient