By Jennifer O’Neill, National Director, Palliative Care, VITAS Healthcare
Suppose your patient with serious illness—COPD, heart failure, cancer, dementia, or other—requires more support than you can provide. Based on their current stage of disease, how do you determine whether home health care, palliative care, or hospice is the optimal referral?
Streamlining the Continuum of Care
Home health, palliative care, and hospice provide different levels of care and have separate eligibility requirements.
Home health is designed to treat an illness or injury and help patients with optimal restorative potential. Skilled home health services include wound care, injections, intravenous or nutrition therapy, and monitoring a patient’s health status. These services are not equipped to provide the higher levels of clinical or psychosocial care that palliative care or hospice offers or meet the complex needs of high-acuity patients.
Palliative care is for patients who are less responsive to disease-directed treatments yet have a prognosis of 18 months or less. VITAS palliative care offers expert case management and care coordination in alignment with patients’ care plans, values, and goals. It ensures patients’ comfort and quality of life while supporting patients’ and primary care physicians’ desired outcomes.
In palliative care, VITAS clinicians help patients recognize where they are in the disease trajectory, available treatment options, and the benefits of hospice care, if appropriate. If the patient has not identified their goals of care, the clinician will initiate ongoing conversations about preferences for care. Advance care planning enables patients to document their goals, including code status/DNR, the use of artificial nutrition/hydration/feeding tube, name a healthcare designee, create a living will, and submit a Physician Orders for Life Sustaining Treatment (POLST) form.
Signs that a patient may need a referral to palliative care include ongoing decline, increased healthcare utilization, and complex requirements at home, among others.
Hospice is for patients who are not responding to disease-directed treatments. If their illness takes the expected trajectory, these patients have six months or less to live. In hospice care, a VITAS interdisciplinary team (including a physician, nurse, aide, social worker, chaplain, volunteer, and others) creates a personalized plan of care for the patient, including psychosocial and spiritual support.
Importantly, VITAS hospice care offers 24/7/365 clinical support, reducing the probability of hospital readmissions or more visits to the ED. Hospice services come to the patient, so the patient can remain in the setting of their choice, whether that is a private home, assisted living community, or nursing home.
The VITAS hospice clinical team provides disease-specific expertise for symptom management and arranges for medications, home medical equipment, and supplies to be delivered to the patient’s home. High-acuity and complex treatments (such as parenteral therapies: antibiotics, TPN light and hydration, inotropes, high-flow oxygen, PT/OT, and speech) are also available.
Hospice is the only one of the three options covered by the Medicare Hospice Benefit (Medicare Part A). If a patient meets hospice eligibility, hospice may be the right next choice for them.
Discussing Care Options with Your Patients
Initiating next-step conversations with your patients and their families is vital. Though it may be easier to discuss home health or palliative care options, goals-of-care conversations help ensure that your patient’s preferences are honored as their illness advances.
Take the time to discuss and ascertain your patient’s goals, wishes, and values for their care. If they have a health crisis, a hospital clinician will likely bring it up instead. Having this discussion with their own healthcare provider who is familiar with them adds comfort to an often-uncomfortable decision.
An annual wellness visit or a post-hospitalization follow-up offers the opportunity to introduce palliative care as an option. When approaching potential hospice enrollment, VITAS can assist you in navigating common misconceptions so your patient can make a timely transition to hospice care.
Making the Right Choice Sooner: Maximize Benefits for Your Patients
Along with choosing the right referral option, when to refer is critical. Often, patients don’t receive palliative or hospice care soon enough. When they don’t, they miss out on the full services that help improve their quality of life.
Palliative care supports longer lengths of stay. The prognosis for palliative care patients is 18 months or less, and support services become available at the diagnosis of serious illness. As the patient declines, hospice becomes a natural and seamless transition.
Yet the transition to hospice is often delayed longer than necessary. According to the NHPCO, the median length of stay for hospice is 17 days1 (a decrease from a consistent 18 days over the last five years). This means most Medicare decedents and their caregivers don’t get access early enough. Because hospice eligibility begins at a prognosis of six months or less, these patients and their families could have received quality-of-life enhancing hospice services weeks, perhaps months, earlier.
Further, studies show that families of patients receiving greater than 30 days of hospice reported the most positive end-of-life outcomes.
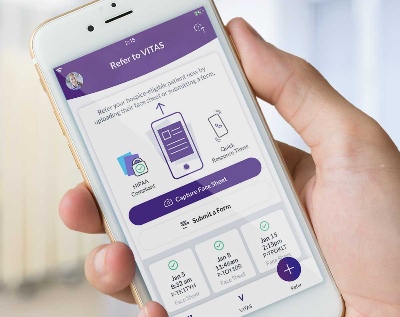
For a palliative care consultation or to refer a patient for hospice, contact VITAS. VITAS also supports you in initiating goals-of-care conversations.
1. NHPCO. (2023). Facts and Figures: Hospice Care in America.