Partnering to Keep Hospice Patients Out of the Hospital
Hospice patients and their family members typically call 9‑1‑1 because they are symptomatic, frightened, or alone—not because they want to go back into the hospital. Most of the time, they are simply searching for additional support.
EMS teams recognize this. Seriously ill patients or their families are among those who call 9‑1‑1 most often. These “frequent runs”:
- Do not benefit the patient
- Put undue pressure on first responders
- Contribute to overcrowding of busy emergency departments
- Result in unnecessary hospitalizations
Because the role of hospice is to ensure in-home support and the most appropriate care possible for patients and families coping with serious illness, collaboration between hospice and EMS benefits everyone. A proactive meeting of the patient, family, EMS, and hospice professional gives everyone an opportunity to assess the situation and get to know one another. That ensures the patient gets the care they need, the caregiver’s fears are allayed, and the EMS is fully informed if they get a call from this address.
VITAS Readmission Prevention Program
An example of this working partnership between hospice and EMS is the collaboration between VITAS Healthcare and Acadian Ambulance Service in Texas. According to Joe Brickner, Vice President of Operations for VITAS in Texas and Kansas, the Readmission Protection Program “allows us to give a higher level of care to our patients and achieve a better level of satisfaction for the patient and family.”
Related: The Value of Hospice in Medicare >
VITAS flags the charts of patients most at risk of going back into the hospital. This determination usually happens at admission, when the patient’s hospice team meets to discuss the physical, emotional, and spiritual needs of the patient and family. Factors include:
- Is the patient full code (no Do Not Resuscitate order in place)?
- Does the patient have a history of going to the ED? Do they verbalize a desire to call 9‑1‑1?
- Does the patient live alone?
- Does the patient or primary caregiver have a high level of anxiety?
- Is this the first time the patient is in a nursing home or assisted living facility following hospitalization?
- Has pain management delivery transitioned from intravenous to oral?
- Does the physician indicate the patient and/or family are struggling with acceptance of the terminal prognosis?
Patients designated high risk receive an introductory visit by the ambulance service’s VITAS-trained paramedics and additional visits and calls from members of their hospice team, including the physician, nurse, hospice aide, social worker, chaplain, and volunteer.
High-risk patients and caregivers are instructed to call Telecare, the VITAS telephone triage system, rather than 9‑1‑1 if they need help. They wear a medical alert system synced with EMS that is activated by the push of a button. When called, Acadian contacts a Telecare clinician, who calls the patient, assesses the situation, and sends the Acadian paramedic, VITAS nurse, and other hospice team members to the patient’s bedside, according to their need.
Under the direction of the VITAS team physician, paramedics are authorized to administer appropriate medications, start IVs, give oxygen, and provide nebulizer treatments and other interventions as needed.
The VITAS nurse determines if the patient’s condition warrants increased visits from the hospice team, Intensive Comfort Care®, or inpatient care. Intensive Comfort Care provides shifts of continuous care in the home until the issue is improved. For severe symptoms that need more specialized or RN care, the paramedics transport the patient to a local VITAS inpatient hospice unit. All of these choices avoid hospital or ED admission.
Meeting the Needs of a Changing Healthcare Marketplace
Partnerships such as the one between VITAS and Acadian Ambulance benefit hospitals, physician groups, insurers, and other healthcare providers by lengthening the patient’s continuum of care.
“This type of program supports the changes in the marketplace and goals of our healthcare partners to keep patients in the most cost-effective setting that aligns with their goals and needs,” explains Brickner. “In the first week of the program, we were able to keep six patients home, preventing them from having to go to the hospital.”
For the patients and families involved in collaborations like this one, the biggest benefit is knowing they are never alone and have the backup support to stay where they really want to be—home.
This article was originally published in October 2016 and updated in September 2023.

Check Hospice Guidelines
Get diagnosis-specific guidelines in our hospice eligibility reference guide.
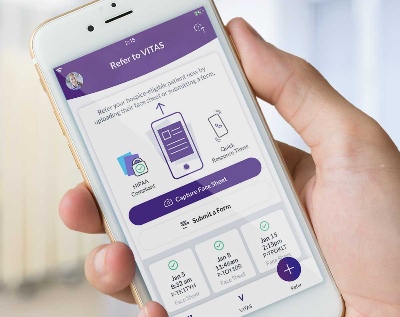
Hospice Guidelines by Diagnosis Refer Your Patient