Palliative Care ‘Void’ Deprives Advanced Lung Disease Patients of Proven Beneficial Care
Palliative care can improve symptoms, patient satisfaction, and quality of life in patients with end-stage disease, yet it remains “a void that needs filling” among patients with advanced lung diseases, according to an article published in the Annals of the American Thoracic Society.
The two most prevalent end-stage lung diseases are lung cancer and chronic obstructive pulmonary disease (COPD), the latter of which was the third leading cause of death in the United States prior to the COVID-19 pandemic and the fourth-leading cause of death worldwide. (The two leading causes of death are heart disease and cancer.)
Hospice Eligibility Guidelines for Advanced Lung Disease & COPD >
Even as treatment of COPD evolves, patients living with this incurable, progressive disease have a heavy symptom burden, including dyspnea, fatigue, cough, and pain. This burden often remains unaddressed at the end of life, write co-authors Rosechelle Ruggiero and Lynn F. Reinke.
“…Strong evidence exists supporting the benefits of integrating palliative care into routine care for persons diagnosed with advanced lung diseases.”-Lynn F. Reinke, PhD, ARNP, VA Puget Sound Health Care System
Patients’ quality of life is also significantly impacted by anxiety—which ranges from 20% in patients whose COPD is stable to 75% in those with severe airflow limitation—and by depression, which averages 40% in all stages of the disease and is greater than 60% among patients requiring supplemental oxygen.
Despite having a higher reported symptom burden than patients with other advanced chronic conditions, less than 15% of COPD patients receive palliative care, according to recent research, with many experiencing high-intensity care as the end of life approaches.
“Patients with COPD are more likely to die in the intensive care unit than patients with lung cancer and are also more likely to receive aggressive measures such as mechanical ventilation at the end of life,” according to Ruggiero and Reinke.
Palliative care is much more than end-of-life care. Palliative care is a clinical specialty that focuses on maximizing a seriously ill patient’s comfort and quality of life. It is therefore appropriate at any point during the COPD trajectory.
Ideally, palliative care should begin before the patient has experienced a significant decline in their well-being or functional status. Palliative care is not synonymous with hospice or end-of-life care—palliative treatments may begin at the time of diagnosis with any serious illness and can continue concurrently with illness-directed therapies.
Benefits of Palliative/Hospice Care
Recent studies found improvements in symptom burden and quality of life in COPD patients—and their family caregivers—with the initiation of palliative/hospice care provided by a multidisciplinary team whose goal is to prevent and relieve suffering, and “attain the best possible quality of life” for those in its care.
Palliative/hospice care provides:
- Management of pain and other physical and psychological symptoms
- Goals-of-care discussions, individualized to align treatment with patient preferences and values
- Coordination and communication between patients and those involved in their care
Initiating palliative solutions into COPD patients’ care plans has also been shown to significantly decrease healthcare system costs, note the authors. “In addition, and more important(ly), patients have a better quality of life when palliative care services and end-of-life discussions are implemented in a timely fashion,” they write.
Barriers to referral to palliative/hospice care include:
- Limited availability of palliative care specialists
- Lack of clinician training in primary palliative care
- No established “trigger” for palliative or hospice care involvement
- Clinician hesitancy in initiating goals-of-care and end-of-life discussions
- Prognostic uncertainty in COPD
“However, discussions about end of life and advanced care planning should not hinge on this prognostic uncertainty,” write the authors, “and these needs can and should be addressed at any time. Many palliative care experts recommend that clinicians start to broach end-of-life discussions at the time of diagnosis.”
This article was originally published in October 2020 and updated in October 2023.
Source: Ruggiero, R., & Reinke, L.F. (2018). Palliative Care in Advanced Lung Diseases: A Void That Needs Filling. Annals of the American Thoracic Society, 15(11):1265-1268. DOI: 10.1513/AnnalsATS.201805-347HP

Check Hospice Guidelines
Get diagnosis-specific guidelines in our hospice eligibility reference guide.
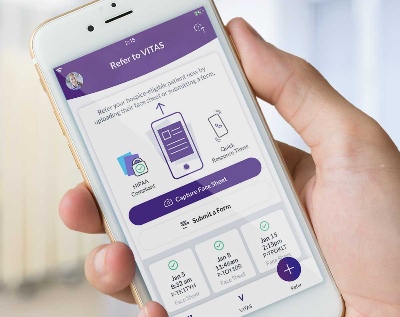
Hospice Guidelines by Diagnosis Refer Your Patient