COVID-19 and Multimorbidity: Exploring the Hospice Option for Care
COVID-19 has transitioned from a life-defining illness to one that exacerbates underlying medical conditions.
According to a study published by the National Center for Biotechnology Information in December 2021, hypertension, cardiovascular disease, and diabetes were among the most common comorbidities in patients who died from COVID-19. More than half of the patients had two or more comorbidities at their time of death.
Though Omicron and other new variants are not as severe, hundreds of people die each day from COVID. -VITAS Chief Medical Officer Joseph Shega, MD
Specific advanced conditions, when combined with COVID-19, are more likely to cause clinical trajectories that trigger the need for end-of-life care. These include advanced heart failure, advanced lung disease, dementia, and cancer.
“With multimorbidity, patients may transition from serious illness to advanced illness,” explains Dr. Joseph Shega, chief medical officer for VITAS Healthcare. “Some of these patients who get COVID-19 will recover to a new lower baseline but still not be hospice-eligible. Others will present exacerbations of underlying disease, with COVID driving further decline. They now become hospice-eligible.”
To provide compassionate care for patients with these trajectories, an interdisciplinary team of hospice clinicians, case managers, social workers, and other care professionals may be the best option.
When Patients Become Hospice-Eligible
The severity of the underlying disease, multimorbidity, and COVID-19 symptoms will together indicate the next stage of medical care. Patients are eligible for hospice care when a physician makes a clinical determination that life expectancy is 6 months or less if the disease runs its expected course.
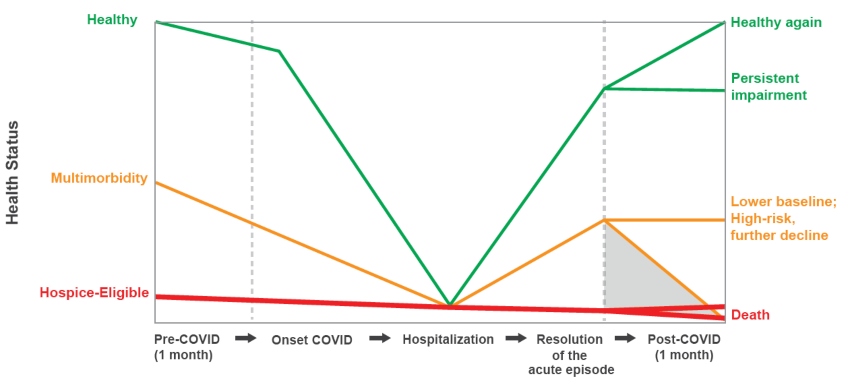
Some patients who get COVID may recover to a lower baseline but not be hospice eligible; others may present exacerbations of underlying disease and become hospice-eligible.
Common Hospice-Eligible Conditions
When these disease states have advanced to the level described below, it may be time to explore hospice care. Only a physician can determine hospice eligibility for a patient.
“Hospitals may see patients who were hospice-eligible before getting COVID, yet not identified as such,” says Dr. Shega. “Once the patients arrive at the hospital with COVID, their condition becomes more apparent. Their physician begins considering a referral to hospice so they can receive the support services they need.”
Advanced Heart Failure
- NHYA class III or IV
- ED visits, hospitalizations within the last 6 months
Advanced Lung Disease
- SOB at rest/minimal exertion on oxygen
- ED visits, hospitalizations within the last 6 months
Dementia
- 3/6 ADL dependency
- Clinical complication in the last 6 months: aspiration pneumonia. UTI, sepsis, multiple pressure ulcers, weight loss
Cancer
- Metastasis
- ECOG 2/3
Case Study: High-Acuity Patient Tests Positive for COVID-19
An 82-year-old is admitted to the hospital for 5 days. The patient was at home and experienced worsening normal ejection fraction (EF) heart failure (HF).
In addition, the patient had a medical history including baseline NYHA Class II-III, long-standing hypertension, diabetes, stroke, and arthritis.
With symptoms including fatigue and a positive COVID-19 test, which was thought to exacerbate heart failure, the patient sought treatment. Despite optimized medical management, the patient’s new baseline moved to NYHA Class III-IV HF.
The patient’s primary care physician referred the patient to VITAS after a post-hospital discharge and a goals-of-care conversation. The patient was admitted to hospice care at home. The VITAS registered nurse on the hospice team ordered oxygen, home medical equipment, and medications.
Related: How The VITAS Open Formulary Benefits Your Patients >
Weekly visits from a nurse, aide, social worker, and chaplain began, along with physical therapy. The team provided higher levels of care and complex modalities. They also adjusted the patient's medications and treatments for comfort.
Through early referral to hospice, the patient received 112 days of care. In total, the hospice team members made 84 visits, managed 8 medications, and provided 5 types of home medical equipment. This high-acuity patient had 10 after-hour visits and Telecare calls. The patient’s level of care changed twice, with 5 days spent in Intensive Comfort Care®.
Why Consider Hospice
Studies indicate that increases in COVID positivity rates are related to a drop in temperature throughout the winter months.1 During this colder season, patients with multimorbidities should remain aware of all of their care options, especially those facing advanced illness.
Nearly 70% of Americans indicate they would prefer to die at home, if given a choice.2 Hospice care can help patients achieve that goal at end of life.
“Though Omicron and other new variants are not as severe, hundreds of people die each day from COVID. The onset of COVID greatly intensifies a patient’s risk. Those with serious illnesses may decline,” says Dr. Shega. “Once deemed hospice-eligible, they can receive the quality of life care they desire from a hospice team.”
- More than 70% of families rate the care as "excellent" when patients received hospice care.3
- Less than 50% of families rate the care as "excellent" when patients died in an institutional setting or with home health services.3
Timely hospice referral ensures patients can receive more care with the VITAS model, ensuring we coordinate with your practice and keep the symptoms of their disease managed.
1Liu, X., Huang, J., Li, C., Zhao, Y., Wang, D., Huang, Z., & Yang, K. (2021). The role of seasonality in the spread of COVID-19 pandemic. Environmental Research, 195, 110874. https://doi.org/10.1016/j.envres.2021.110874
2Kaiser Family Foundation/The Economist Four-Country Survey of Aging and End-of-Life Medical Care (2017). Conducted March 30–May 29, 2016.
3Teno J.M., Clarridge B.R., et al. (2004). Family perspectives on end-of-life care at the last place of care. JAMA, 291(1):88–93
Upcoming Webinars for Healthcare Professionals

Tips for Effective Goals-of-Care Discussions
Conduct more effective goals-of-care discussions with your patients by using this conversation starter guide.
Download Now Clinicians: Receive Our Newsletters
