VITAS Respiratory Therapists Help Patients Breathe Easy with Compassionate Research
Ask any hospice care professional about why they entered the field; you’ll likely hear something about improving quality of life or making a difference for a patient.

Anton Lukcevic, VITAS respiratory therapist in Chicago
Most of these improvements, while integral to the mission of hospice, are incremental, intimate and noncurative: a couple more “good” days than last week, the renewed strength to eat a meal with loved ones, fewer bed sores, etc.
Sometimes, however, the work of hospice professionals can uncover opportunities to improve quality of life for more patients than any one person could have imagined.
Such is the case for respiratory therapists Anton Lukcevic and Vikki McCoy of VITAS in Chicagoland: Their recent research into aerosolized/nebulized morphine could change the way respiratory issues near the end of life are treated—and help countless patients breathe more easily.
Anton, Vikki and their three University of Chicago colleagues found that morphine delivered via nebulizer more effectively treats dyspnea and other respiratory complications with fewer side effects compared to other delivery methods.
A paper detailing their findings, “Oxygen Therapy and Aerosolized Morphine to Treat Symptomatic Dyspnea During Palliative and Hospice Comfort Care,” was published in Symbiosis.
‘The Sickest Patients in the House’
“Respiratory issues can be very distressing to a patient at the end of life, and it’s often very hard for others to watch,” Anton says. “We see the sickest patients in the house, so to speak.”
He’s certainly seen a lot. After 52 years as a respiratory therapist in acute care, critical care and hospice settings – 12 of which have been with VITAS – Anton has witnessed the full breadth of respiratory ailments and symptoms that can afflict a patient, from labored breathing to the notoriously unsettling “death rattle."
“Vikki and I are in this to help people, and it’s been very rewarding.”
Up to 70 percent of all hospice patients experience respiratory issues near the end of life, namely in the form of dyspnea – or shortness of breath. Dyspnea can stem from a variety of physiological conditions, but it may also be exacerbated by physical manifestations of anxiety.
Many patients report dyspnea to be more distressing than physical pain, so managing both a patient’s respiration and anxiety is crucial to avoiding a cascading intensification of symptoms.
Used to treat many common symptoms encountered in hospice, morphine is a proven and reliable relief option for patients with dyspnea. But side effects such as drowsiness, nausea and constipation routinely affect patients taking morphine, potentially increasing their distress.
‘It Works!’ – Without the Side Effects
To obtain the detailed data necessary for their research, the study’s authors spent three years working with 110 patients and their care teams in the inpatient unit at Chicago’s St. James Hospital. Nurses administered the morphine nebulizer treatments, then recorded patients’ vital signs, lung sounds, oxygen saturation levels and verbal responses before and after the treatments.
The researchers found that nebulized morphine – morphine delivered via oxygen line to the patient’s respiratory tract – relieved dyspnea faster than oral administration and with no apparent side effects.
“It was kind of surprising,” Anton says. “A lot of patients said they were breathing better right away, within 10 to 15 minutes of getting the nebulizer treatment.”
Anton read aloud a few statements from patients:
“Wow, I’m breathing better.”
“I feel so much better.”
“It works!”
‘We’re Going to Breathe a Little Bit on This’
Between patients’ feedback and their vital signs, the study shows promise for countless patients choosing between breathing issues and the side effects of traditional morphine delivery. But Anton says he, Vikki and the university research team have more work to do before their study prompts lasting change.
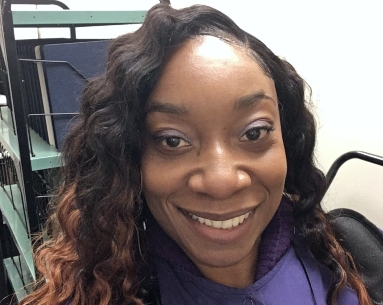
Vikki McCoy, VITAS respiratory therapist in Chicago
The University of Chicago – Anton’s alma mater and a key partner of VITAS in delivering end-of-life care – has already approached Anton and Vikki about a follow-up double-blind study, in which some patients would receive a placebo while others receive morphine, but the details and methodology are still being finalized.
That’s fine by Anton, who’s ready for a well-deserved rest.
“We’re going to breathe a little bit on this first,” he says. “It was a massive undertaking – but well worth the time invested.”
Anton didn’t become a respiratory therapist for the research; he followed that path to make people feel better. In fact, the face-to-face connection with a patient is his favorite part of his job. But there’s still joy in knowing his study could improve the care and comfort level for hospice patients whom he’ll never meet.
“Vikki and I are in this to help people, and it’s been very rewarding in that way,” Anton says. “Believe it or not, I’m 72 years old and I don’t plan to retire anytime soon. I still love what I’m doing.”

Choose a Career with VITAS
We offer a variety of full-time, part-time and per-diem employment opportunities. Employees earn competitive salaries and have the flexibility to choose a benefits package suitable to their own needs and lifestyle.
See Current Opportunities
